“The fact of homelessnessamong mentally ill people is compelling enough,” Dr. Dennis Culhane was saying. “The fact that we can demonstrate the cost-neutrality of housing them makes it even more compelling—even for fiscal conservatives—to take action.”
Culhane, associate professor of social welfare policy, was referring to a recent study which concluded that providing “supportive housing” for mentally ill homeless people essentially pays for itself. Since on any given day there are an estimated 110,000 homeless people with severe mental illness in this country—and the cost of providing shelter, jail, and hospital services for them costs an average of $40,499 a year (at least in New York City, where the study was carried out)—the implications of that conclusion are considerable.
The study was undertaken by Culhane and two other researchers at Penn’s Center for Mental Health Policy and Services Research, Stephen Metraux G’98 and Dr. Trevor Hadley, professor of psychiatry. It examined data on 4,679 homeless people with “severe mental disorders” who were placed in New York City supportive housing between 1989 and 1997, and merged that data with administrative data on their use of public shelters, hospitals, Medicaid-funded services, veterans’ inpatient services, state psychiatric inpatient services, state prisons, and the city’s jails. About half the people studied were placed in supportive housing between 1993 and 1997 through a public initiative by the state and city of New York, known as the New York/ New York agreement.
The study—whose results are being published in Housing Policy Debate, a journal of the Fannie Mae Foundation—compared those in supportive housing with homeless people not placed in housing.
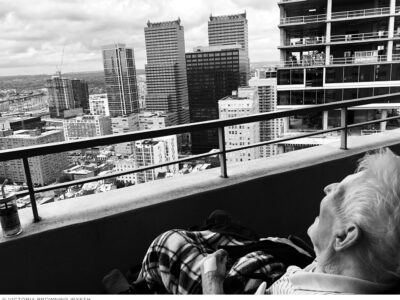
Unlike shelters or transitional housing, says Culhane, supportive housing is “basically private rental housing in an efficiency apartment,” in which “services are provided by mobile teams that include medical personnel as well as social workers.” The social workers’ job, he adds, “is to make sure that if people’s health starts to decline, or their symptoms recur, they get proper attention, their bills are paid, and they’re progressing with their own personal objectives.”
While the yearly cost for each housing unit was estimated at $18,190, the study noted, “placement in housing through the program was associated with a reduction in service use of $16,282 per housing unit per year.” Overall, the initiative (which included some community mental-health residences as well as supportive-housing units), “resulted in a net cost of $1,908 per unit per year,” and that figure would have been even lower had supportive-housing units alone been used. “In other words, 95 percent of the costs of the supportive housing (operating, service, and debt-service costs) are compensated for by collateral service reductions attributable to the housing placement.”
“A considerable amount of public dollars is spent essentially maintaining people in a state of homelessness,” Culhane points out. “What this study proves is that by putting those same dollars into supportive housing, the solution can pay for itself.”
Although one could imagine a community putting up some resistance to supportive housing, Culhane says that the benefits outweigh the drawbacks.
“Because they involve full rehabilitation of previously neglected buildings, the multi-unit projects tend to stand out as improved housing in the neighborhood,” he says. “They’ve even been found to help property values. The units stand out and, over time, the people tend to be embraced by the community.” Especially since the housing is not just for the mentally ill but for a “mix of tenants and incomes, which helps subsidize the units.”
Culhane first approached the state and city agencies that deal with New York’s homeless population in 1994, but it took him nearly five years to get authorization to examine the data. “You’re dealing with very confidential records,” he explains, “so many assurances are required.”
He chose New York because it had a “major initiative” in supportive housing,” he says, but “we would very much like to replicate the study in Philadelphia” now that the city has several hundred such units in service.
The New York study has been “very well appreciated and absorbed by policy-makers and community activists,” he says. “People still want to see if the same thing holds in other places. Congress and the federal agencies have been very interested consumers of this study. We’ve done a couple of briefings for a federal agency’s staff, and [in late June] I testified in the House of Representatives, at a committee hearing, to present the results.”
He thinks that the odds are “pretty good” that more supportive housing will, in fact, be built, though as the study points out, “it remains a major public-policy challenge to shift funds from one set of purposes (health, jails, prisons) to another (housing or housing support services).” Two years ago, Congress mandated that 30 percent of money spent on the homeless “must go to permanent housing for the chronically homeless,” Culhane notes. But while that funding is provided by the Department of Housing and Urban Development (HUD), “health services are paid for by HHS [Health and Human Services] and the states.” Since the agencies that save money by housing the homeless are HHS and the states, he adds, “the big question is: Will HHS and the states put up the money for services for this housing that HUD has created? HUD can provide 90,000 units of housing over the next 10 years. But health services actually cost more than housing.” (According to the study, the average cost of those services was approximately $9,100 per unit per year, and the reductions in inpatient hospital costs attributable to the housing intervention were $8,260 per year.)
What goes unmentioned, of course, are the “intangible benefits” to homeless people. “We couldn’t quantify them, using government records,” Culhane acknowledges. “But the biggest benefit is that people have a place to live, and have privacy and a place to imagine their future and to live from. That’s something we take for granted.”