

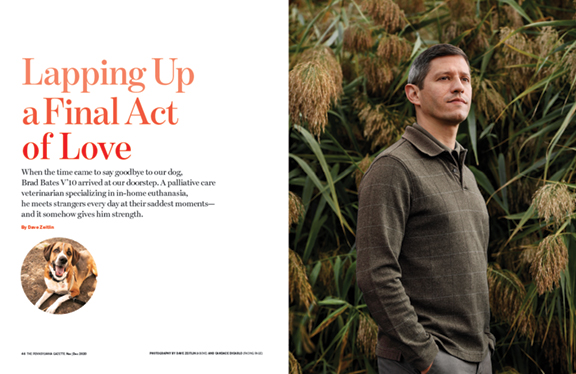
When the time came to say goodbye to our dog, Brad Bates V’10 arrived at our doorstep. A palliative care veterinarian specializing in in-home euthanasia, he meets strangers every day at their saddest moments—and it somehow gives him strength.
By Dave Zeitlin | Photography by Candace diCarlo (top) and Dave Zeitlin
“Is it the day?”
I awoke to my six-year-old son’s somber voice in my ear, as he snuggled up next to me and disappeared under the comforter, the same way our dog used to when she was able to gallop up the stairs and fearlessly launch herself onto our bed. Now, she couldn’t even stand on her own and had to be carried down the front steps of our house to pee.
I groggily turned to my son, eyes opening.
“Yeah, buddy. It’s the day.”
For any pet owner, there’s no avoiding the day. It’s forever looming, from the joyful day you bring home your furry friend, to the pull-your-hair-out days your pup pees in the house, to the blissful days there’s nowhere else you’d rather be than curled up against soft fur. A dog’s lifespan is cruelly short; maybe that’s why they squeeze in so much love and excitement while they’re with us.
My wife, Lauren, and I thought we’d be prepared for it. As our dog’s health began to rapidly decline—which aligned with the beginning of the COVID-19 pandemic, giving us an extra layer of quarantine sadness and worry at a time when so many others were dealing with far greater grief—we assured Sammie’s veterinarian that we wouldn’t hold on for longer than we should. We huddled in a stairwell one Sunday afternoon in July, the vet on the phone, our two young kids yelling in the background, when we agreed that, after months of appointments and prescriptions, there was little more that could be done for her.
After 11 years, it was time to say goodbye to our first pet.
So what comes next?
Our vet doesn’t make house calls and hauling a virtually immobile 80-pound dog into the car and to a veterinarian’s office seemed a particularly terrible way to go—especially for an animal whose longstanding anxiety made her shake uncontrollably at the vet on even her best days. And because of our kids, it would have been a logistical challenge for Lauren and me to both be with Sammie during any procedure out of the house. So we were recommended to reach out to Brad Bates V’10, a mobile veterinarian with the Philadelphia branch of Lap of Love, a national veterinary hospice and in-home euthanasia service.
Dr. Brad, as he’s called on the company’s website, would come into our house, euthanize our dog with a quick and painless injection, and take her away in his van to be cremated. The whole thing would last no longer than 45 minutes.
It initially felt strange and almost jarring that a vet who, over the course of many years, had come to know all of Sammie’s quirks and tendencies would cede end-of-life care to a vet who didn’t know her at all. But it still felt like the right thing to do—or so we hoped.
I called Lap of Love on a Monday and got an appointment for the following day. The woman I talked to on the phone was very sympathetic and helpful, but questions still swirled in my brain after I hung up, from the weighty to the mundane. Should we request her ashes back? How will Dr. Brad manage to get Sammie from our house to his van? Will he find parking on our narrow city street? Do you put an appointment like this on your Google calendar?
And the hardest question of all: How do we brace a six-year-old for such a profound moment in his young life?
When the day arrived, we had already had the conversation with our son. We explained to him that Sammie’s health issues had gotten to the point that putting her to sleep was the kindest thing to do. We expected him to perhaps push back as he had in previous talks, pleading we find medicine to make her better. This time, he only hugged us and cried, finding solace that maybe she’d be able to run again in doggie heaven.
Dr. Brad would tell me later that he generally advises his clients to be honest with their children—and that kids, even younger ones, should be there during the euthanasia since “there’s nothing scary about it,” nothing that might traumatize them. “Unfortunately we’re not prepared to deal with death in this country and families don’t often prepare kids unless they have a death in the family,” he says. “For me, the easiest answer is they should all be present. If a pet teaches us about responsibility and love, they can also teach us about life and death.”
We likely would have had our six-year-old by our side for the procedure but that day he had summer camp, a happy distraction. As he got ready in the morning, he shared his blueberry muffin with Sammie, who took a few nibbles and declined the rest. By then, she had mostly stopped eating—even her favorite people food. It was one of the telltale signs that we were making the right call, along with her severely enlarged liver, her reluctance or inability to walk outside, and the pressure wounds that formed as a result. Of course, we still questioned it. Dr. Brad calls it a catch-22: people only make the decision to end their pet’s suffering because they love them, but that same love keeps them from wanting to say goodbye. Sometimes he counsels them, or tries to offer a little affirmation that they’re doing the right thing. “Honestly a lot of what we do falls under social work or therapy,” he says, adding that some people express relief if he finds something else that might be wrong with the pet that they hadn’t known about before.
After Sammie ate what would be her final bites of food, our son had a quick catch with his younger sister, squeezing in a little silliness before the painful moment of saying goodbye to a friend he had his whole life. Then, he put on his shoes, kissed Sammie on the head, and walked to the camp bus stop with Lauren.
After they left, I tried to gently tell our daughter, who had just turned three, that Sammie would be going away. “She’s going to live in her school?” she asked excitedly, before turning her attention to Sesame Street. Her youthful innocence was a relief; having one child grapple with the gravity of life and death was more than enough for one day.
Time passed slowly until the 11 a.m. appointment. We looked through old photos and videos of Sammie, laughing at how she howled along with ambulance sirens or tilted her head to the rhymes in the Dr. Seuss book Green Eggs and Ham. Lauren apologized to her for all the times she got upset about her peeing on the hardwood floor.
Dr. Brad arrived right on time. We grabbed our masks to put on and welcomed him inside. His tone was gentle, and he kneeled beside Sammie, letting her sniff his hand. Instinctively, I scratched her beneath her chin, making sure she was OK. As she’d gotten older, Sammie had grown increasingly nervous when strangers entered the house. But this time, she simply laid her head back down, as if she knew why this one had come. It’s probably silly, but I like to think she felt relief in that moment, grateful that her pain and confusion would soon disappear. Or maybe that was just me. In a moment in which I was about to lose a wonderful companion of more than a decade, it seemed surprising how much gratitude and warmth I felt toward someone I had just met.
How careful does he have to be with every word and action? Is it possible to make small talk? Does he change his approach at all based on a person’s emotions? Even through tears, I could not beat back my curiosity about how Dr. Brad approaches a job that entails meeting people for the first time at one of their saddest moments, before exiting their lives almost just as soon as he entered it.
“We don’t know what we’re going to be exposed to,” he admits. “We don’t even know the patient. … I greet people exactly the same as I always do, and then you almost have to read them and mirror them.”
Occasionally, he says, someone will mark his visit as a celebration of life with music playing that’s so upbeat that he “almost has to bring them into the moment.” On the other end of the spectrum, a pet owner might be so grief-stricken (a lot of times because they’ve experienced other loss, or don’t have much of a support system to fall back on) that they express anger and frustration about the procedure. “That’s the worst thing for us to hear,” says Dr. Brad, who communicates often with other Lap of Love vets from around the country. “It devastates us. I always tell the new doctors to focus on what you did for the pet. Sometimes there are people who you will never, ever make feel good. It could go almost perfectly technically, but they saw something that they didn’t want to see, and they will never be at peace. There’s nothing you can say that can take that memory away.”
More often than not, however, Dr. Brad meets people who “are the same,” he notes. “They grieve the same. They live the same. The way they comfort their loved ones is the same. The way they teach their kids is the same.” When he steps into someone’s home, it doesn’t matter what politicians they like or what cable news channel they watch, which, “in this world of division we have in this country,” has been one of the most rewarding parts of his job.
“There’s something to be said about people who love animals—they tend to be compassionate,” he says. “It’s amazing how much love they give doctors despite the fact they’re losing a family member. They really don’t bring us into their sadness. If anything, the most common thing we probably hear is: ‘I’m sorry I’m crying in front of you.’”
I expected to cry, but I think the amount of tears surprised me. It started days earlier and happened at strange times, like when the Trader Joe’s cashier asked how my day was going, or while I was frying up bacon because it was the only thing Sammie would eat the night before the Lap of Love appointment. By the time Dr. Brad arrived, Lauren and I had a hard time even finishing sentences without choking up.
After he gave her a heavy sedative and prepared the pentobarbital, a seizure medication that most veterinarians use to euthanize pets, he asked a little more about Sammie. I said she was 11, and he told us how big dogs really start to slow down once they hit double digits. I’m sure he knew that we knew that, but it made us feel a little better all the same.
“She wasn’t even supposed to be a big dog,” I sniffled in response.

When we rescued her from a Delaware County foster home, where she had arrived from a kill shelter in North Carolina, Sammie was a 10-week-old mutt that looked as a beagle might. The vet told us she’d probably end up to be 30 pounds. She grew into an 80-pound beast. Part beagle … part horse? Whenever someone stopped us on the street to ask us what kind of dog she was—which happened often, usually with an air of incredulity—I’d generally mutter something along the lines of, “We’re not really sure—some kind of giant beagle mix.” She packed all that weight into a lean and athletic package, too. She galloped through shallow water. She ran circles around other dogs at the dog park. One time, she sprinted across a frozen lake in Vermont—a sight equally terrifying and majestic.
Now that same dog was meekly curled up on her bed underneath an open window at the front of our house, as Dr. Brad shaved a few clips of hair off of her hind leg to ready the injection. A light breeze rolled in, and the branches of our neighbor’s plum tree across the street swayed. The muffled sounds of Vampirina could be heard from the basement where our daughter was obliviously watching one of her new favorite Disney shows. (Trying to find a show or movie that would keep her attention long enough so she didn’t come upstairs just at the moment her dog died had been a uniquely excruciating case of remote control pressure.) A Philadelphia Parking Authority worker walked by in headphones, talking loudly. A car horn blared. “Well, it’s the city,” Dr. Brad said, and we all tried to muster smiles.
As he injected the pentobarbital into Sammie’s vein, Lauren stayed by Sammie’s face and held her paw. I kept my head on her heart, listening to it slow, quietly saying “Good girl” over and over. By the time Dr. Brad used his stethoscope to check for a heartbeat, I already knew.
“She’s at peace, guys,” he said.
Dr. Brad started working at Lap of Love two years after graduating from Penn’s School of Veterinary Medicine, initially on a part-time basis. By then, he had done a few in-home euthanasias as a general practice veterinarian, and “already knew it was nicer to do these procedures at home.” And he noticed that even though there was a lot of demand for it, few vets do it. So his part-time job at Lap of Love gradually evolved into a full-time one, “because it was basically just more necessary” than practicing general or emergency veterinary medicine.
Before long, he came to love it. Yes, it can be emotionally draining, but “the fulfilling nature” of the work has sustained him. “I think people don’t realize how much love we are exposed to during visits, compared to regular visits in a clinic,” he says. “We always tell vets to do this work for a while before you judge it.” During a euthanasia at a clinic, the pet might be nervous and the family uncomfortable, but “when you go to someone’s house, everyone is more at peace,” he says. “We come in and we meet people who literally love their pets like we love our pets. That connection is immediate, and that connection is real.”
Meeting those people at their own homes “gives us power,” he adds. “Then we see a pet that’s peaceful, and that gives us a lot of strength.”
A distressing moment in his own life has also fueled his work. While at Penn, Dr. Brad nursed a sickly kitten named Laker with a severe respiratory infection back to health and cared for him. But when Laker was two, he developed lymphoma and Dr. Brad made the difficult decision to put him down, with the help of a colleague. Robbed of more time with his pet, he still remembers how difficult it was to let someone else take Laker away after the euthanasia. “In my head,” he says, “I don’t think I was ever going to let go. It’s such an uncomfortable feeling. It’s probably the worst feeling next to making the decision.”
Dr. Brad learned from his mentor, Dani McVety, a cofounder of Lap of Love (which, since its opening in 2009, has grown into the largest network of veterinarians dedicated solely to end-of-life veterinary care, with more than 90 of them situated around the country), never to ask someone if they’re ready for the euthanasia part because “they’ve already made the decision.” He’s also learned through years of experience—including his own feelings of letting Laker go—not to ask people how much time they’d like with the pet afterwards “because that’s such a hard question.”
But they do offer some alone time following the euthanasia. We learned that when Dr. Brad left our house to pull his van around the block so he could double-park right out front, while Lauren and I solemnly looked at Sammie’s lifeless body for what felt like an eternity. Only later did we learn that he was repeatedly thwarted by construction and road closures, eventually having to back down our narrow street. Without having a static hospital, those are some of the logistical complications he encounters on many of his visits to homes around the Philadelphia region. “Sometimes, people have 100-pound dogs in high-rises and there’s no parking and tons of people walking,” he says. “That is emotionally difficult, and logistically difficult.”
Luckily we live on a quiet block (occasional nearby construction aside), but one question still gnawed at me as I assisted Dr. Brad in lifting Sammie onto the stretcher that he had brought inside from his van.
“Do you cover her head?” I asked, looking at the doggie-designed blanket atop the stretcher.
“Not usually,” he responded. “But if a kid might walk by …”
We decided to keep Sammie entirely covered, and then I helped Dr. Brad awkwardly maneuver the heavy stretcher down our front steps. For Lauren and me, this was probably the toughest part—the idea of someone taking away a pet that we first brought home 11 years ago. In a lot of ways, we were mourning a period of time in which we had no idea a tiny puppy sprawled on our laps in the car would turn into a huge hound who would ride shotgun with us on a journey through a marriage, an apartment, two houses, and two kids.
As we lifted the stretcher into the back of the van, our neighbor with the plum tree stood just inside his screen door and gave a salute. Perhaps in non-COVID times, I’d have offered Dr. Brad a friendly embrace before he drove our dog to his garage, where the crematorium they work with would pick up the body. (We opted for a communal cremation, rather than a private one in which we’d be able to keep her ashes. The paw print and clips of fur that Lap of Love made for us were lovely remembrances on their own.) Those parts of interactions have of course changed, much to his chagrin. Before the pandemic, “sometimes I’d come in and someone would just start crying and falling into my arms,” he says. “They don’t even know me. It’s the sight of me and they know who I am. We can’t do that now. That’s really difficult. The best thing you can do is get a hug from someone at the end of an appointment, or a really heartfelt handshake.”
With only a wave, I began to walk away, toward our quieter, emptier house. But for some reason, I decided to quickly turn around to tug on the blanket a bit so it wasn’t covering Sammie’s head anymore. Then, before the van door slammed shut and Dr. Brad drove down our block and around the corner, I gave her one last ear scratch for the road.





