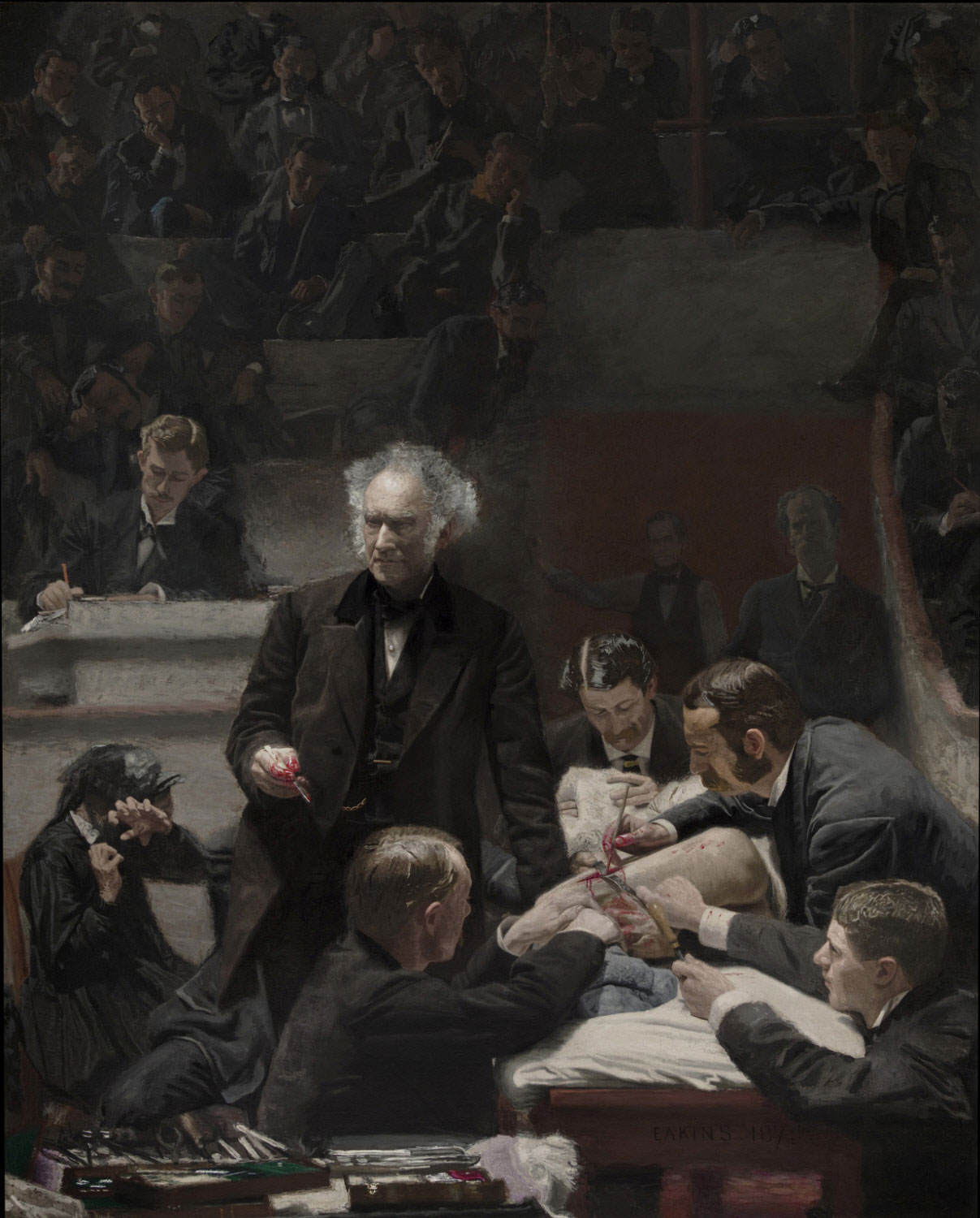
The Gross Clinic by Thomas Eakins, 1875.
As a fine arts minor at Penn, Jaclyn Gurwin C’11 M’15 learned how to look deeply at a work of art and not just see it, but truly observe it.
When she continued on to medical school, she discovered how useful—and rare—that training was. Doctors need to be expert observers, but it’s a skill most medical schools don’t specifically teach.
“I saw how much art had an impact on my medical training,” Gurwin says. “I felt like because of all the art classes I had taken, I saw things a little differently.”
She wondered if teaching other medical students to look closely at artworks could improve their powers of observation. That’s where the study came in.
Backed by a small research team—including Gurwin, another medical student, and several doctors—plus funding from the Perelman School of Medicine, the study launched in 2014. It sent 18 first-year Penn medical students to the Philadelphia Museum of Art for six hour-and-a-half training sessions led by museum educators. Another 18 students received a free membership to the museum but no formal training.
Before and after the course, all 36 students took tests that asked them to describe three different types of images: art images, retinal photographs, and external eye clinical photographs.
The results appear in the current issue of Ophthalmology medical journal (January 2018). We talked with Gurwin about her findings as the study’s lead author and what they mean for medicine and future students. The conversation has been condensed and lightly edited for clarity.
What set your research apart from previous studies that have looked at similar themes?
We realized that there weren’t many formal studies that looked at the effects of training students in art observation alone. Also, most of the other studies were not very rigorous in that they weren’t randomized controlled trials. They mostly had students take courses and then reflect on their experience, and there wasn’t formal testing. We were also the first study, to my knowledge, that looked at fine art’s effect on ophthalmological observational skills as opposed to just medical observational skills in general.
And what did you discover?
Not only did the students in the art training group improve their art observational skills compared to the control group—which we would assume—but they also improved their medical and ophthalmological observational skills as well. Just learning these techniques of observing and describing in the fine arts world was enough to translate to improved medical observational skills.
Why do you think that happens?
I think it works because art observation is almost the same as the observation we’re doing in medicine. When you’re looking at a piece of art, you’re using terms like line and color and perspective, and we’re doing the same thing. When I describe a patient’s retina who’s coming in for a diabetic eye exam, I may say that the retina has, for example, three small, round intraretinal red spots in the inferotemporal periphery.
Just in that one sentence, I’m using terms that are describing the quantity, the size, the shape, the depth, the color, the distribution. It’s encapsulating all those same terms that you’re using when you’re describing artwork. It’s not that we’re necessarily training students to look at something in particular when they’re looking at an image, but rather to fully look at an image to describe exactly what they’re seeing.
How does being a better observer help a doctor or future doctor provide better care?
I think great doctors are inherently great observers because without observation, you’re not able to develop a diagnosis or a treatment decision. If you’re looking at, say, a freckle in the retina, you have to be able to observe certain characteristics to know if they’re concerning for melanoma. If you aren’t looking carefully, a potentially life-threatening disease could easily be missed.
So what did the PMA classes entail?
They taught a method of systematically going about observing works of art. A lot of people are used to going through the whole museum and looking at each painting for maybe 30 seconds to a minute. This was very different. Over an hour-and-a-half period, they sat by maybe two or three paintings and shouted out what they saw. People were still seeing new things at the end of the 30 minutes.
They also learned vocabulary terms like line and color and shape, and they focused on being flexible in your thinking and changing your viewpoint based on what other people were saying. All those things were based on initial observations when looking at artwork. We found that it was very similar to what we do in the medical field: we make observations when we’re examining a patient, and then based on those observations, we come up with a differential diagnosis and a treatment plan.
Did the works they looked at include The Gross Clinic?
I think that might have been the first session, actually. I think they wanted to get them excited with something medical-related. They also looked at works that were totally abstract with no people in them at all, and others that were more focused on people and emotion.
You proved that this training is applicable in your field of medicine, but do you think it could help people who practice other types of medicine, too?
I think this is applicable to all fields of medicine and surgery as well. Probably the most applicable would be fields that are very visual—ophthalmology, dermatology, radiology—but even if you’re a primary care physician or a psychiatrist, observation is extremely important. I think it’s possible that [art observation] could help people learn anatomy and just be better visual learners.
In medical school, we’re just sort of expected to know how to do [this observation]. We really don’t get trained in it, and we’re more expected to memorize terms instead of saying, ‘Okay, instead of jumping to the diagnosis here, just tell me what you’re seeing in basic language.’ It doesn’t need to be in medical terminology. Just to be able to describe something to someone is really helpful in figuring out what’s going on.
What are you hoping to see come out of the results from your study?
I hope that more medical schools will look at this and think about how they can incorporate other fields into medical training—whether it’s art or music or something else—to really enhance the medical education system. I think that’s something that we’re just at the beginning of right now, but I think it’s going to grow and get even bigger.
Is Penn still offering this art observation class?
Yes, the pilot study that we did is now an elective for first-year medical students. Ideally, I’d like to see it expand even more, because I think it would be great for residents as well.
Are there other aspects of this that you’re still hoping to explore?
We hypothesized that not only would this help ophthalmological and medical observational skills, but that it would also somehow help with emotional recognition and empathy. I believe that the first step in being empathetic is to be able to observe. Are there tears in someone’s eyes? What is their body language? Are they slouched over? Are they sitting erect? All these different things, which are simple observations, allow you to recognize emotion, and then you can respond with empathy. I think there needs to be more work done to fully figure out the best way to utilize art in training people to be more empathetic, but I think there’s something there. We’re working on that.
—Molly Petrilla C’06

