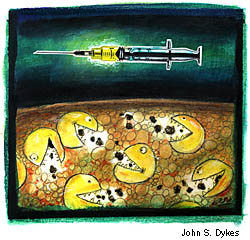
Researchers at the University of Pennsylvania Medical Center have made important advances on two fronts of the war against cancer. In one, a team working with colleagues from the National Cancer Institute (NCI) has found a quick new way to boost the immune system’s cancer-fighting forces — in other words, to make a cancer vaccine. The procedure involves
transforming the body’s abundant monocytes — immune cells circulating
in the blood — into battle-ready dendritic cells, which play a key role
in stimulating the immune system. While most people think of vaccines
as something administered to patients before they contract a disease,
cancer vaccines are designed to spur the immune system into attacking
existing tumors.
“Our procedure could be used to produce vaccines against cancers,
including breast cancer, colon cancer, and melanoma,” says Dr. Brian J.
Czerniecki, assistant professor of surgery in the School of Medicine.
He and Dr. Peter Cohen of the NCI will conduct a clinical trial with
melanoma patients next spring. “We plan to kick-start the immune system
of these patients by giving them melanoma-antigen-labeled dendritic
cells,” explains Czerniecki. “These cells will have the instructions to
activate T cells to find the melanoma tumor and work at shrinking it.”
Czerniecki and his colleagues reported their findings in the October 15
issue of the Journal of Immunology.
In the other discovery, a team led by Dr. Wafik S. El-Deiry,
assistant professor of medicine and genetics, has identified a
“death-receptor gene” that goes by the name “KILLER/DR5” and responds to
chemotherapy and radiation by killing cancer cells. That discovery,
says El-Deiry, “gives us new insight into how cancer cells treated with
chemotherapy and radiation die.”
When the researchers introduced extra copies of the gene into
colon- and liver-cancer cells in laboratory experiments, cell growth was
completely stopped. According to El-Deiry, who is also an assistant
investigator with the Howard Hughes Medical Institute, that finding
suggests that “substitution or reactivation of KILLER/DR5 in cancer
cells may be a reasonable strategy for killing those cells.”
The team’s findings appeared in the October issue of Nature Genetics.