Training health workers to stop HIV in postwar Liberia. No need to sugarcoat.
By Peter Ehrenkranz
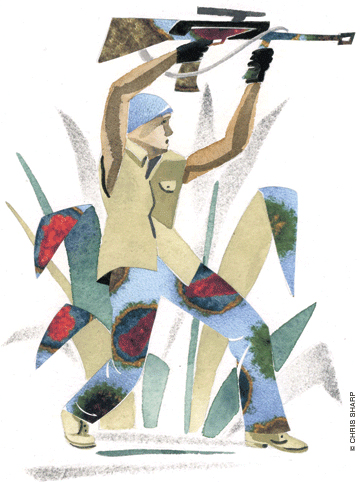
“Liberians have seen enough soldiers. I think we should take these pictures out of the presentation.”
Two other Western-trained doctors and I are putting together a training module for HIV treatment teams in Liberia. Jerry, an assistant professor of infectious diseases at an American university, is objecting to the military metaphors typically used to describe the course of the HIV virus. The virus is the attacker. The CD4 cell is the immune system’s first line of defense—the Marines. The virus invades the body’s home territory, taking over the very “factories” where immune cells are created. Instead of making new Marines, the factory is used to replicate the attackers.
Michael and I shrug. Jerry, who volunteered with the Peace Corps in Liberia in the 1980s, has a much broader perspective on the country than we do. Back for the first time since his original stint of service, he has seen the effects of 14 years of civil war. Upon his recent return to the town where he had volunteered, he found that one of his good friends had been “taken away” during the fighting and had never returned.
So maybe he’s right—a gratuitous reminder of the war in the middle of an HIV lecture is something we can do without. I lean toward the computer and change the color of the “soldier’s” uniform from green to blue, and write police on his chest. Perhaps this way we can remind our audience of the importance of supporting and respecting the nascent Liberian National Police instead.
The lecture’s primary goal is to introduce a new way of delivering care to HIV patients. Since there are fewer than 40 doctors in the country, we’re trying to shift much of the patient-care load onto auxiliary staff—nurses, midwives, counselors, physician-assistants, and the like. To pull it off, we have to make sure the lectures are accessible to everyone among this wide range of participants. That means keeping scientific jargon to a minimum and focusing on basic concepts. Just as crucial, it means being mindful that all of these people have just been through the war and are fighting to trust their government—and each other—again.
After editing out the military rhetoric, I email the slides to Dr. Abraham Borbor, head of the HIV clinic at JFK, the largest government hospital in Liberia. Dr. Borbor has agreed to help us teach the HIV lectures. There are few other Liberians with more experience treating the disease. Even when he left the country during the last years of the war, he took up work in an HIV clinic in Tanzania, returning home after the new government took power.
Almost as important, he has a gift for teaching. He understands the call-and-response style that his countrymen seem to enjoy. I won’t get a chance to review the lecture with him prior to the workshop, but I’m confident that he’ll be able to engage the audience and teach the material better than we could.
This creativity and motivation tends to be more evident in those who had the means to leave during the war—even if just for a little while, like Dr. Borbor. Most of the people we will be teaching stayed through the worst parts of the conflict, many going to work even when salaries were not being paid, when their homes were between onslaughts by different rebel factions, when neither the United Nations or the United States could commit to saving the country from itself. After surviving that chaos, it is a wonder to me how they seem to be so willing to move forward, even to forgive and forget. More than once, a coworker of mine has pointed out a particularly ruthless former rebel commander from the car window in the same manner I would use if I happened to spy an especially mean teacher from junior high.
I know that the workshop participants will welcome me warmly, and for the most part, be open to my suggestions, but many of them cannot quite figure out why I care enough to be here. Most of the international NGOs that came to this part of Africa for the adrenaline rush of providing care in a conflict setting are leaving. What’s more, Liberians have been trained to survive, to make decisions only when necessary, to avoid questioning their superiors. The Americans that take jobs like mine want to push them to do things better, faster, and more efficiently—not just to “check boxes.” But I don’t want to just help them do their work, I want to raise their expectations. They should have a working X-ray machine, drugs to treat their patients, and a government that will keep them in supply. As Médicins Sans Frontières and the International Rescue Committee decamp for more dangerous territory, soon Liberians will be in charge and must improve their situation themselves. But recent experiences have made Liberians fearful of change, or perhaps just deeply skeptical that it can happen.
A week later, the rough beginning of our training session gives me my own cause for doubt. The workshop starts with a last-minute change of venue and the discovery that our participants have less experience than we thought. More than half of them are unfamiliar with how to use a table of contents. Even fewer are comfortable navigating patient-care flowcharts to determine appropriate courses of action.
We’re behind schedule, sweaty, and lost in the weeds when Dr. Borbor takes his place at the front of the stiflingly hot room, trying to wake people up after a typically heavy Liberian lunch.
“You see this picture here?” he asks the group, pointing to a slide with an artist’s rendering of the virus attacking a CD4 cell that he’s evidently added on his own. “This is the virus attacking the base of the immune system.”
Michael and I exchange raised eyebrows from across the room. Hadn’t we changed the slides to avoid these sorts of metaphors?
“You all know what it’s like to be under attack,” Dr. Borbor continues. “There’s lots of shooting going on!” He holds out his hands as if he’s cradling a rifle and yells: “Bam-bam! B-b-b-b-b-bam!”
Everyone laughs at his impersonation of a soldier.
Dr. Borbor goes on with great animation. Doctors and nurses need to encourage their patients to take the antiretroviral medicines consistently, he says. This is how patients can control the attackers. But beware, he adds, because the virus is never completely dead—it is just hiding until it has another chance to come out.
“What did you do when you heard bad stuff going on outside?!” he asks.
Laughter erupts from the audience again: “We hid!”
“And when there was no more shooting?” Again, he cradles his imaginary rifle. “You went and looked for food!”
The laughter intensifies. Dr. Borbor pretends to peek around a corner and look for bad guys.
“Well to the virus, the medicines are the bad stuff. They are going to find a place to hide until they sense that there’s quiet outside. Tell your patients to take their medicine every day so the virus stays quiet!” Many of the participants are laughing so hard they are crying. Some of them are literally falling out of their chairs. And as Dr. Borbor looks out over his latest pupils, their laughter crescendos and turns into cheers.
Peter Ehrenkranz GM’05, recently a Robert Wood Johnson Clinical Scholar at the University, is the Clinton Foundation HIV/AIDS Initiative’s medical director in Liberia.




